Awards
IHEA has three awards:
- The Adam Wagstaff Award for Outstanding Research on the Economics of Healthcare Financing and Delivery in Low- and Middle-Income Countries;
- The Arrow Award for the best published health economics paper; and
- The Di McIntyre Student Paper Prize for the best paper by a Masters or Doctoral student.
- Adam Wagstaff Award
- Arrow Award
- Di McIntyre Student Paper Prize
Adam Wagstaff
3 May 1959 – 10 May 2020
IHEA President 2016 – 2017
This award was established by colleagues and friends in memory of Adam Wagstaff and was funded through ‘Friends of Adam’ crowdfunding. The prize is awarded to the best IHEA congress paper on the economics of healthcare financing or delivery in a low- or middle-income country(ies) (LMIC) that is written and presented by a researcher from a LMIC. It reflects Adam’s lifelong commitment to these issues and to promoting equity in LMICs.
Applications for this award are submitted through the IHEA Congress abstract submission process.
About the Adam Wagstaff Award
- Award Eligibility Criteria
- FAQs on Eligibility Criteria
- Submission & Selection Process
- Nature of the Award
- Most Recent Awardee
- Committee
- Funding & Governance
- Previous Awardees
- This award is intended for early career researchers (ECRs)/recent graduates, not those currently studying. Students are encouraged to submit an entry for the annual IHEA Student Paper Prize.
- To be considered for the Adam Wagstaff Award, the ECR must have an abstract accepted for oral presentation at the IHEA congress. You must indicate your interest in being considered for this award during the abstract submission process.
- The paper must focus on the economics of healthcare financing or delivery in a LMIC (this can include a country defined by the World Bank as a middle-income country until not more than a year ago, that is now classified as a high-income country). The research should be policy-relevant in that it should provide insights into how to improve healthcare financing or delivery. Papers with an equity focus are encouraged.
- The first author of the paper (or corresponding author where authors are listed alphabetically) and presenter at the congress must be a citizen of a LMIC (using the World Bank country income classification). Co-authors on the paper are not restricted to LMIC citizens.
- The main author and presenter at the congress must have submitted their doctorate or have completed their doctorate within the last 7 full-time equivalent years.
- To be considered for the award, a full paper must be available three months before the congress and be submitted with a personal statement of 500 words outlining your future career plans at the time of application.
- Submitters should be willing to commit to contributing to health economics in LMICs if they win this award. This could take the form of mentoring researchers with very limited experience, co-supervising a (post-)graduate student, serving on the Award Committee in future, or related activity, depending on the skills and preferences of the Awardee.
Can I submit a paper that analyses global data, so includes low-, middle- and high-income countries? No, only papers that have a specific focus on LMICs will be considered.
Can a paper that considers theoretical or methodological issues be submitted? Usually not, unless there is a very specific focus on LMICs (e.g. development of an innovative methodology for health care financing or delivery research to address data constraints in LMICs).
Can an economic evaluation paper be submitted? Generally not. As the focus of the award is on the economics of health care financing or delivery, only economic evaluations that compare alternative service delivery options and/or include a budget impact analysis of services that address a major burden of disease in LMICs will be considered. Papers that focus purely on the effectiveness of health care interventions or an economic evaluation of a very specific clinical intervention are not eligible.
If I graduated 8 or 9 years ago, but had maternity leave and worked part-time for a year afterwards, will my paper be considered? Yes, as long as the full-time equivalent working period after graduation is no longer than 7 years at the time of application.
If I am a citizen of a LMIC, but am currently living and working in a high-income country, will my paper be considered? Yes, as long as the paper focuses on LMICs and your intention is to continue undertaking research focused on LMICs.
Those from a low- or middle-income country with an accepted abstract, on the economics of healthcare financing or delivery in a LMIC, for the next IHEA congress will be invited to submit a full paper for review by the selection committee three months prior to the congress. The selection criteria are comparable to those used for the Arrow Award and the Student Prize, which focus on the importance of the contribution of the paper and appropriateness and innovation in methodology.
The award includes a certificate and a cash prize, which will be presented during one of the plenary sessions of the congress. The session in which the award-winning paper is presented will be highlighted as a special session and the presentation will be followed by discussant input. In addition, the winner will be invited to present at the World Bank’s Health Finance Forum.

Rym Ghouma
Do Providers Contribute to Socioeconomic Inequalities in Health Care? An Audit Experiment in Tunisia
Rym Ghouma is a Health Economist and Research Fellow at the Institute for Research and Information in Health Economics (IRDES) in France. Her research focuses on applying economic theory and empirical tools to better understand provider behavior and the determinants of healthcare quality in both the public and private sectors. She is particularly committed to informing health policy debates in Tunisia—her home country—and in other low- and middle-income settings, particularly those in the Middle East and North Africa (MENA) region.
Currently, she is engaged in research on hospital financing, performance, and quality of care in the French healthcare system, with the aim of applying these insights to other contexts.
Rym graduated in 2024 with a PhD in Health Economics from the London School of Hygiene & Tropical Medicine (University of London) and has a Master of Public Affairs (MPA) from Sciences Po Paris. She also earned an MBA at the South Mediterranean University (SMU) in Tunis and a B.A. in Economics at ESSEC Business School.
In addition to her research, Rym has lectured at Sciences Po Paris and consulted for international organizations such as the Organisation for Economic Co-operation and Development (OECD) and various United Nations agencies. Prior to her research career, she held several managerial positions in the healthcare industry across the Middle East, Africa, and Europe.
Rym’s diverse background and experience inform her commitment to supporting equitable and effective health system reforms in both developing and developed settings.
The Adam Wagstaff Award Committee is also pleased to announce Honorable Mentions to two other papers submitted for the 2025 IHEA Congress:
Chenyuan Liu: Decentralized Policymaking and Market Distortions: Evidence From China’s Drug Formulary Design
Vishnu Prasad Sapkota: Coping (more or less) with Health Shocks: a Longitudinal Perspective on Financial Protection from Nepal
Members of the initial Award Committee were selected to include at least one close colleague of Adam’s from long-term collaborative research projects; at least one of Adam’s colleagues from the World Bank with expertise in this sub-field; and at least one researcher with expertise in the sub-field who is based in or affiliated with a LMIC institution. The Committee members, in alphabetical order, are:
Augustine Asante, University of New South Wales and Centre for Health Financing and Systems Innovation Africa
Edwine Barasa, KEMRI-Wellcome Trust Research Programme
Damien de Walque, World Bank
Eeshani Kandpal, Center for Global Development
Hong Liu, Renmin University of China
Anne Mills, London School of Hygiene and Tropical Medicine
Owen O’Donnell, Erasmus University
Rudi Rocha, São Paulo School of Business Administration
Aparnaa Somanathan, World Bank
Winnie Yip, Harvard University
Funds raised through ‘Friends of Adam’ crowdfunding are ring-fenced for this award, with auditing and IHEA Board oversight of revenue and expenditure as for all IHEA finances. In addition, there will be biennial reporting to the Award selection committee for additional oversight.
We would like to acknowledge the generous contributions of the following individuals and groups, as well as several anonymous contributors, towards this Award:
Ronald Akehurst, Sarah Alkenbrack, Elaine Baruwa, Marcel Bilger, Caryn Bredenkamp, Terkel Christiansen, Jorge Coarasa, Daniel Cotlear, Agnes Couffinhal, Damien de Walque, Tim Ensor, Patrick Eozenou, Tim Evans, Deon Filmer, Emanuela Galasso, John Giles, Karen Grépin, Mutsa Gumbi, Reem Hafez, Emmanuel Jimenez, Andrew Jones, Eeshani Kandpal, Beth & Mead King Over, Felicia Knaul, Joseph Kutzin, Soonman Kwon, Gabriel Leung, Elisa Liberatori Prati, Jui-fen Rachel Lu, Di McIntyre, David McKenzie, Owen O’Donnell, Ceyla Pazarbasioglu, Kjeld Pedersen, Eugenio Prati, Stella Quimbo, Marisol Rodriguez, Miriam Schneidman, Gil Shapira, Richard Smith, Peter Smith, Sally Stearns, Sandy Tubeuf, UPSE Health Econ Lab, Eddy Van Doorslaer, Tom Van Ourti, Marcos Vera-Hernandez, Michael Woolcock, Vasoontara, Yiengprugsawan, and Winnie Yip
Giancarlo Buitrago, The Effect of Outpatient Cost-Sharing on Population-Level Mortality: Regression Discontinuity Design Evidence from Colombia
Radhika Jain, Private Hospital Behavior Under Government Health Insurance in India
Kenneth J. Arrow
23 August 1921 – 21 February 2017
This annual award was established in honor of Kenneth Arrow and in recognition of the influence of his seminal paper from 1963 “Uncertainty and the welfare economics of medical care”. It recognizes excellence in the field of health economics, with the award presented to the author(s) of the paper judged to be the best paper published in health economics in English in the award year.
The deadline for submissions for the 2025 Arrow Award is January 19, 2026. Submit online by completing the form and uploading the paper using the “Submit a Paper” button.
About the Arrow Award
- Submission & Selection Process
- Most Recent Awardees
- Committee
- Previous Awardees
- Submit a Paper
Deadline: Annually in mid-January
IHEA’s Arrow Award was created to recognize excellence in the field of health economics with the Award presented to the author or authors of the paper judged to be the best paper published in health economics in English in the award year. The Award was set up in honour of the late Kenneth Arrow and in recognition of the influence of his seminal paper from 1963 “Uncertainty and the welfare economics of medical care”. Professor Arrow was involved in the creation of the Award and he presented the inaugural prize in 1993.
The Award is made every year. The Terms of Reference of the Committee and guidelines for scoring of short-listed papers, can be viewed here.
Nominations for the Arrow Award from members of IHEA are encouraged and should be submitted below.
The 33rd Arrow Award for the best paper in health economics is awarded to:
Alsan, M., Durvasula, M., Gupta, H., Schwartzstein, J. and Williams, H., 2024. Representation and extrapolation: evidence from clinical trials. The Quarterly Journal of Economics, 139(1), pp.575-635.
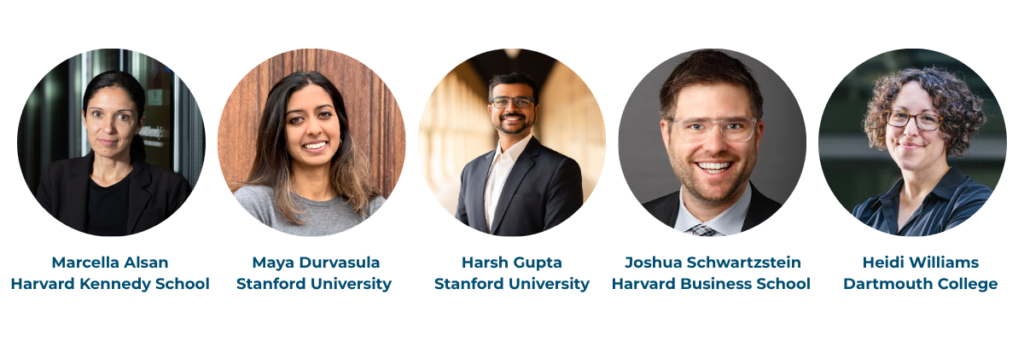
The Arrow Award Committee proudly recognizes the authors of this innovative paper that examines the consequences and causes of low enrollment of Black patients in US clinical trials. The authors introduce a theoretical model of similarity-based extrapolation. The model predicts that the relevance of clinical trial results for a group not only depend on the average benefit from a trial, but also on whether the group is properly represented in the trial. The framework predicts that physicians and patients update their beliefs about drug efficacy more when clinical trial samples closely match their own demographic group.
In survey experiments the authors find that physicians, especially those caring for more Black patients, are more willing to prescribe drugs tested in more representative samples. The effect size is substantial enough to potentially close existing gaps in prescribing rates for new medicines. Similarly, Black patients shown evidence from representative trials are more likely to believe the drug would work for them and express increased willingness to participate in future trials and trust in researchers.
Despite these benefits, the study’s model and evidence suggest that underrepresentation persists because those who have historically benefited from medical innovation are less costly to enroll, reinforcing disparities in evidence generation. The findings underscore the importance of representative clinical trials for improving health equity and trust and suggest policy interventions to address persistent underrepresentation in clinical trials.
We congratulate the authors on the publication of this important paper.
Chair: Marcella Alsan, Stanford University
Marika Cabral, University of Texas
Gabriella Conti, University College London
Apostolos Davillas, IZA/Institute of Labor Economics
Bruce Hollingsworth, Lancaster University
Xiaoyan Lei, Peking University
Aurélia Lépine, University College London
Hsienming Lien, National Chengchi University
Nhung Nghiem, Australian National University
Edward Okeke, Pardee RAND Graduate School
Erin Strumpf, McGill University
Judit Vall Castelló, Universitat de Barcelona
Stephanie von Hinke Kessler Scholder, Bristol University
Marcia Weaver, University of Washington
Edward N. Okeke, 2023. When a doctor falls from the sky: The impact of easing doctor supply constraints on mortality. American Economic Review, 113(3), pp.585-627.
Sendhil Mullainathan and Ziad Obermeyer, 2022. "Diagnosing Physician Error: A Machine Learning Approach to Low-Value Health Care." Quarterly Journal of Economics, 137(2): 679-727.
Andrew Goodman-Bacon, 2021. "The Long-Run Effects Of Childhood Insurance Coverage: Medicaid Implementation, Adult Health, And Labor Market Outcomes." American Economic Review, 111(8):2550-2593.
Nava Ashraf, Oriana Bandiera, Edward Davenport, and Scott S. Lee, 2020. "Losing Prosociality in the Quest for Talent? Sorting, Selection, and Productivity in the Delivery of Public Services" American Economic Review, 110(5): 1355–1394.
Tatyana Deryugina, Garth Heutel, Nolan H. Miller, David Molitor, and Julian Reif, 2019. The Mortality and Medical Costs of Air Pollution: Evidence from Changes in Wind Direction. American Economic Review , 109 (12): 4178-4219. DOI: 10.1257/aer.20180279.
Marcella Alsan and Marianne Wanamaker. Tuskegee and the Health of Black Men. Quarterly Journal of Economics133(1): 407-455, 2018.
Marika Cabral. 2017. Claim Timing and Ex Post Adverse Selection. Review of Economics Studies84(1): 1-44.
Martin Gaynor, Carol Propper, and Stephan Seiler. 2016. Free to choose? Reform, choice and consideration sets in the English National Health Service. American Economic Review106(11): 3521-3557.
Eric Budish, Benjamin N. Roin and Heidi Williams. 2015. Do firms underinvest in long-term research? Evidence from cancer clinical trials. American Economic Review105(7): 2044-2085.
Jeffrey Clemens and Joshua D. Gottlieb. 2014. Do Physicians' Financial Incentives Affect Treatment Patterns and Patient Health? American Economic Review104(4): 1320-49.
Jonathan T. Kolstad. 2013. Information and quality when motivation is intrinsic: evidence from surgeon report cards. American Economic Review,103(7):2875-2910.
Amy Finkelstein, Sarah Taubman, Bill Wright, Mira Bernstein, Jonathan Gruber, Joseph P. Newhouse, Heidi Allen, Katherine Baicker, and the Oregon Health Study Group. 2012. The Oregon Health Insurance Experiment: Evidence from the First Year. Quarterly Journal of Economics, 127(3):1057-1106
Randall D. Cebul, James B. Rebitzer, Lowell J. Taylor, Mark E. Votruba. 2011. Unhealthy Insurance Markets: Search Frictions and the Cost and Quality of Health Insurance. American Economic Review,101(5):1842-71
Carol Propper and John Van Reenen. 2010. Can pay regulation kill? Panel Data Evidence on the Effect of Labor Markets on Hospital Performance. Journal of Political Economy, 118(2): 222-273
Kate Ho. 2009. Insurer-Provider Networks in the Medical Care Market. American Economic Review,99(1):393-430
Hanming Fang, Michael P. Keane, and Dan Silverman. 2008. Sources of Advantageous Selection: Evidence from the Medigap Insurance Market. Journal of Political Economy, 116(2): 303-350.
Amitabh Chandra and Doug Staiger. 2007. Productivity Spillovers in Health Care: Evidence from the Treatment of Heart Attacks. Journal of Political Economy, 115: 103-140.
Kevin M. Murphy and Robert H. Topel. 2006. The Value of Health and Longevity. Journal of PoliticalEconomy, 114(5): 871-904.
Gary S. Becker, Tomas J. Philipson, and Rodrigo R. Soares. 2005. The Quantity and Quality of Life and the Evolution of World Inequality. American Economic Review, 95(1):277-291
Edward Miguel and Michael Kremer. 2004. Worms: Identifying impacts on education and health in the presence of treatment externalities. Econometrica, 72(1); 159-217.
Kenneth Chay and Michael Greenstone. 2003. The Impact of Air Pollution on Infant Mortality: Evidence from Geographic Variation in Pollution Shocks Induced by a Recession. Quarterly Journal of Economics, 118(3):1121-1167.
Anne Case, Darren Lubotsky and Christina Paxson. 2002. Economic Status and Health in Childhood: The Origins of the Gradient. American Economic Review;92(5): 1308-1334.
Willard G. Manning and John Mullahy. 2001. Estimating Log Models: To Transform or Not to Transform? Journal of Health Economics, 20(4): 461–494
David M. Cutler, Mark McClellan and Joseph P. Newhouse. 2000. How Does Managed Care Do It? Rand Journal of Economics, 31(3): 526–548
Will Dow, Tomas J. Philipson and Xavier Sala-i-Martin. 1999. Longevity Complementarities Under Competing Risks. American Economic Review,89(5):1358-1371.
Donna B. Gilleskie. 1998. A Dynamic Stochastic Model of Medical Care Use and Work Absence. Econometrica, 66(1): 1-45.
Ching-To Albert Ma and Thomas G. McGuire. 1997. Optimal Health Insurance and Provider Payment. American Economic Review,87(4): 685-704.
Daniel Kessler and Mark McClellan. 1996. Do Doctors Practice Defensive Medicine? Quarterly Journal of Economics, 111(2): 353-390.
Martin Gaynor and Paul Gertler. 1995. Moral Hazard and Risk Spreading in Partnerships. RAND Journal of Economics, 26(4): 591-613.
Jonathan Gruber. 1994. The Incidence of Mandated Maternity Benefits. American Economic Review, 84(3): 622-641
Phillip Cook and Michael Moore. 1993. Drinking and schooling. Journal of Health Economics, 12(4): 411-429.
Richard Hirth. 1992. Nursing Home Quality: Roles of Information and Ownership (Unpublished paper)
Applications for 2026 are now closed!
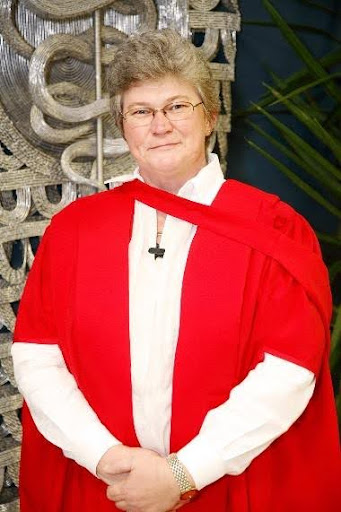
Di McIntyre Student Paper Prize
IHEA Executive Director 2016-2026
This annual award, previously known as the IHEA Student Paper Prize, was renamed the Di McIntyre Student Paper Prize in 2026 to acknowledge the important and lasting impact of IHEA’s previous Executive Director, Di McIntyre, particularly on engagement with early career researchers.
The award recognizes excellence by students in the field of health economics and is awarded to the master’s or doctoral student paper judged as best in the award year.
About the Di McIntyre Student Paper Prize
- Prize Eligibility Criteria
- Submission & Selection Process
- Nature of the Prizes
- Most Recent Winners
- Committee
- Previous Winners
- Submit a Paper
- Applicants must currently be studying (full- or part-time) at a higher education institution, at either Masters or Doctoral level. In addition, students who completed their studies in the year previous to the call for submissions qualify, as long as the paper was written while registered as a student.
- Papers can be published or unpublished, but must be in comparable format to a published paper in Journal of Health Economics or Health Economics, of maximum length 8,000 words (excluding abstract, tables, figures, references and any appendices).
- Papers should be in English.
- A cover letter is required, signed by the student’s supervisor, confirming that the student’s contribution is at least 75% and outlining the nature of the student’s contribution and that of any co-authors (conceptualization, analysis, writing etc.).
- Previous winners are not eligible.
The International Health Economics Association (IHEA) is pleased to invite submissions for the Annual Student Paper Prize in Health Economics. Submissions should include a copy of the paper (preferably .pdf) and a cover letter, signed by the supervisor, outlining the student’s contribution (which should be at least 75%) and that of any co-authors. As an international association, IHEA highly encourages those from around the globe to share this call with their networks and submit their papers for consideration.
A student is defined as someone currently studying (full- or part-time) at a higher education institution, at either Masters or Doctoral level. In addition, students who have completed their studies in the year previous to the announcement qualify as long as the paper was written while registered as a student.
Papers can be published or unpublished, but must be in a comparable format to a published paper in the Journal of Health Economics or Health Economics, and have a maximum length of 8,000 words (excluding abstract, tables, figures, references and any appendices). Papers should be in English. Previous winners are not eligible.
Papers will be reviewed by an International Committee chaired by Professor Tinna Laufey Ásgeirsdóttir (University of Iceland) and co-chaired by Shiko Maruyama (Jinan University, Guangzhou).
Please submit your paper and cover letter, and complete the form, at the bottom of this page.
The Prize will be complimentary registration for the next IHEA Congress to present the paper in a Student Prize Special Organised Session, a cash prize and the offer (if the author wishes, and the paper is unpublished) of potential fast track publication in Health Economics, subject to Editorial approval.
The papers in 2nd and 3rd place will receive a small cash prize and complimentary registration for the next IHEA Congress. They will be invited to give brief presentations at the IHEA Congress Student Prize Special Organized Session. All prize winners will also receive a certificate.
The 2025 Student Paper First Prize was jointly awarded to:

Marie-Anne Boujaoude
This study provides the first Australian equity weights derived from public preferences (n=2400), quantifying the degree of health inequality aversion by income group, Indigenous status, and geographic location. The findings suggest that most Australians are willing to prioritize health gains to disadvantaged groups. These empirically derived inequality aversion parameters can support more equity-informative economic evaluation through Distributional Cost-Effectiveness Analysis (DCEA).

Hidetoki Nakayama
This paper examines whether policy can enhance public trust in government. Using Japan’s age-based COVID-19 vaccination policy, we conduct a regression discontinuity design to identify the causal impact of receiving a vaccine on trust in government. Our findings suggest the importance of policy benefits in building public trust.
Honorable mention go to the runner up:

Deivis Guzman
Using nationally representative data and a multivalued treatment framework, this paper finds that monthly payments significantly improve diet quality and diversity relative to bi-monthly transfers. The results highlight the role of payment frequency in consumption smoothing and behavioral responses, offering new evidence to inform the design of social protection programs and advancing our understanding of how income timing shapes consumer choices.
The prize winners will present their papers at a special session of the 2025 IHEA Congress in Bali.
Many thanks to all those who submitted papers for consideration, and to the Prize Committee for all their hard work. The next call for submissions will be issued later in 2025.
The Student Prize is sponsored by the Canadian Centre for Health Economics.
Chair: Tinna Ásgeirsdóttir, University of Iceland
Co-Chair: Shiko Maruyama, Jinan University, Guangzhou
Mehdi Ammi, Carleton University
Ronelle Burger, Stellenbosch University
Michal Horný, University of Massachusetts Amherst
Brenda Gannon, University of Queensland
Flavia Mori Sarti, University of São Paulo
Jacob Novignon, Kwame Nkrumah University
Alfredo Paloyo, University of Wollongong
May Ee Png, Oxford University
Timothy Powell-Jackson, London School of Hygiene and Tropical Medicine
Peter Sivey, University of York
Sally Stearns, The University of North Carolina at Chapel Hill
Raf van Gestel, Erasmus University
Matthew V. Zahn (Johns Hopkins University): “Entry and Competition in Insurance Markets: Evidence from Medicare Advantage”
AND RUNNERS UP
Priscilla Kandoole (University of York): “Consumption Smoothing and Welfare Effects: Mtukula Pakhomo Social Cash Transfer Program”
Yuki Kanayama (Keio University): “Unintended Effects of Delayed Marriage on Women’s Attitudes toward Intimate Partner Violence: Evidence from Cambodia”
Yashaswini Singh, Johns Hopkins University, “Can Private Equity Buy Referrals? Evidence from Multispecialty Physician Practice Acquisitions”
AND RUNNERS UP
Vera Zabrodina, “Timing Moral Hazard under Deductibles in Health Insurance”
Benedikt Janzen, “Temperature and Mental Health: Evidence from Helpline Calls”
Henry Cust, LSHTM, "Trading HIV for Sheep: An estimation of the sexual behaviours response of female sex workers to Tabaski in Senegal”
AND RUNNERS UP
Hanifa Pilvar, Queen Mary University of London, “Changing physicians’ incentives to control the C-section rate: Evidence from a major health care reform in Iran”
Domininkas Mockus, University of Illinois, “The Effect of Immigration on the Living Arrangements of Elderly Natives”
Elaine De Gruyter, Monash University. Altruism born of suffering? The impact of an adverse health shock on pro-social behaviour.
Jill Furzer, University of Toronto. ADHD Misidentification in school: Causes and mitigators.
AND
William Schpero, Cornell University. The long run effect of Medicaid on receipt of public assistance.
Monica Aswani, University of Alabama at Birmingham, Differential Impact of Hospital and Community Factors on Medicare Readmission Penalties.
Mujaheed Shaikh and Tobias Muller (Austria/Switzerland),Your retirement and my health behavior: Evidence on retirement externalities from a fuzzy regression discontinuity design.
Raf Van Gestel, University of Antwerp, and Tobias Müller, University of Lucerne, Does My High Blood Pressure Improve Your Survival? Overall and Subgroup Learning Curves in Health.
Joseph Dieleman, IHME, University of Washington, Measuring the displacement and replacement of government health expenditure.
Ranjeeta Thomas, University of York, Conditional cash transfers to improve education and health: an ex ante evaluation of Red de Protección Social, Nicaragua
Pedro Rosa Dias, University of York. Inequality of opportunity in health: evidence from a UK cohort study.
Stephanie von Hinke Kessler Scholder, University of Bristol, Maternal employment and overweight children: does timing matter?
Teresa Bago d’Uva, University of York, Latent class models for utilization of health care.
Paula Gonzalez, Universidad Pablo de Olavide, Sevilla, Should physicians’ dual practice be limited? An incentive approach.
Nazmi Sari, Boston University, Do managed care and competition improve quality? Evidence from US hospital markets.
Mathias Kifmann, Universität Konstanz, Community rating in health insurance and different benefit packages.

